Leukaemia and Lymphoma
Malignancy is a disease of rapidly growing cell types. Cells that are dormant and not going through the cell cycle do not accumulate the 6-7 mutations that are needed to produce malignant transformation of a cell. Leukocytes are one such cell type, with the bone marrow producing enormous numbers of white cells daily. In all other cell types, malignancy causes cancer – the growth of a solid tumour. But because the white cells are released into the blood stream, solid masses are not necessarily a feature of haematological malignancy.
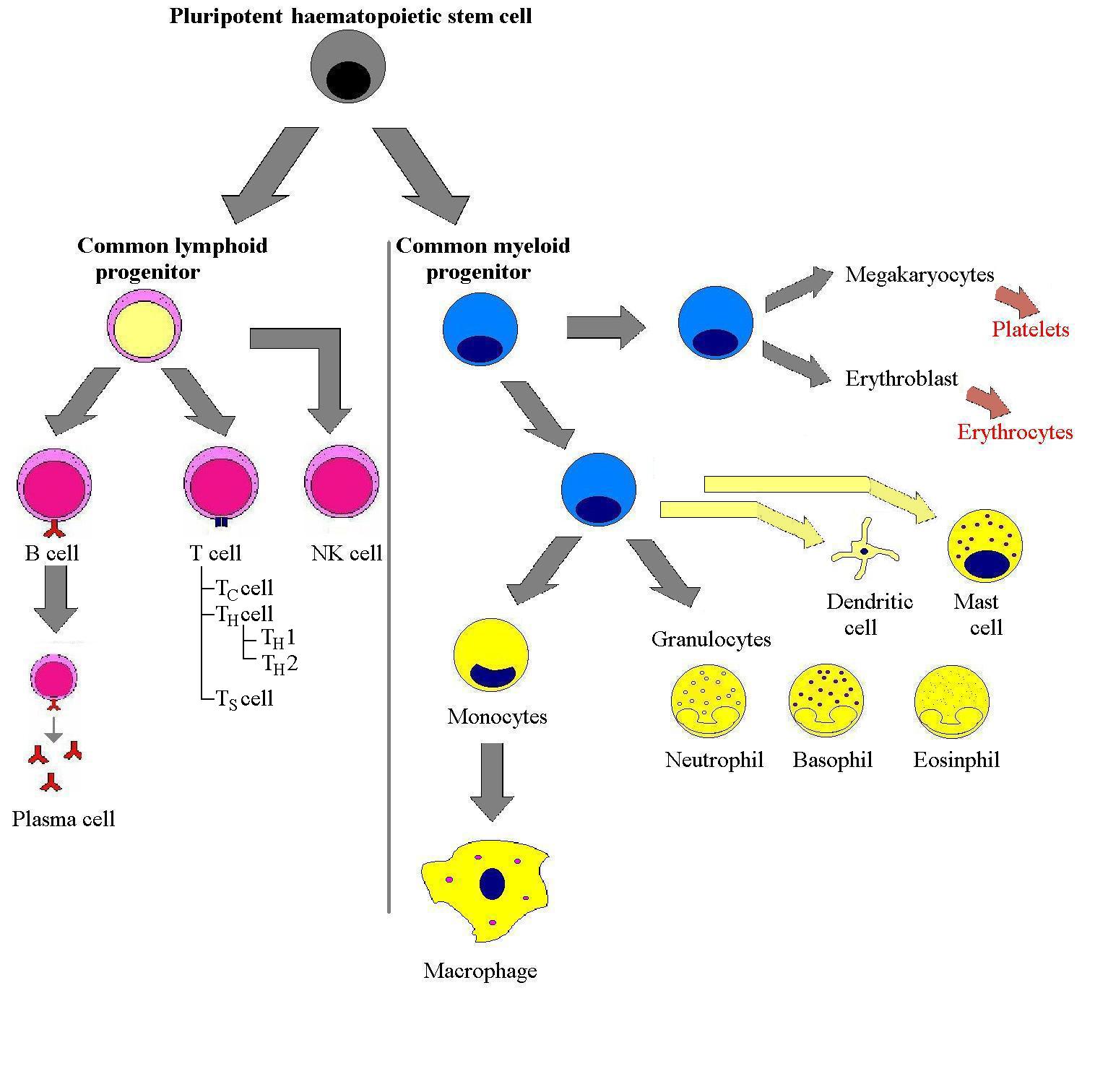
The leukaemias are categorised in two ways: by their cell lineage and time course of the disease. Leukaemias are classified as lymphoid or myeloid, reflecting the origin of the malignancy: either within the lymphoid cell line or the myeloid cell line. Lymphoma is malignancy that arises within secondary lymphoid organs from lymphoid cells (lymphocytes and their precursors). As such, lymphoma and lymphoid leukaemia are essentially the same disease process, differentiated mainly by the site of the malignacy.
The other major means of categorising leukaemia is into acute or chronic. The course that the leukaemia follows s dependent on the stage of the cell development at which the malignancy arises. A stem cell or poorly differentiated cell that becomes malignant will cause an acute leukaemia, whereas a mature leukocyte-originating transformation results in a chronic course. The pathogenesis of leukaemia is primarily one of bone-marrow failure. Normal blood cell production is sequestered into producing leukaemic cells. The poorly differentiated cells are fast growing and hence give rise to acute disease whereas the chronic leukaemias are caused by mature cells that accumulate very slowly. Commonly, in acute leukaemia blast cells are visualised on a blood film. These blast cells are immature white blood cells which are normal in bone marrow but not in peripheral blood.
The signs and symptoms of leukaemia can be deduced from a knowledge
of the normal function of bone-marrow derived cells. This normal function
is hindered by the sequestration of bone marrow by the disease process. Anaemia
and thrombocytopenia (and therefore bleeding) are seen due to the loss of
erythocyte and megakaryocyte production which occurs because they are derived
from the same stem cell as the white blood cells. High rates of infection
are seen due to the loss of a normally functioning immune system. The other
group of symptoms - lymphadenopathy, splenomegaly and hepatomegaly - is due
to the infiltration of secondary lymphoid organs.
Acute Lymphoblastic Leukaemia (ALL)
Chronic Lymphocytic Leukaemia (CLL)
Acute Myeloid Leukaemia (AML) and
Chronic Myeloid Leukaemia (CML)
Lymphoid Leukaemias and Lymphocytes.
The World Health Organisation classifies ALL into three different
types: 1. Precursor B ALL; 2. Burkitt cell leukaemia and 3. Precursor T ALL.1
From an immunological perspective there are leukaemias that arise from each
stage of B-lymphocyte development:
· Lymphoid progenitor - Acute lymphoblastic leukaemia
· Pre-B cell - Pre-B cell leukaemia
· Naïve B cell - Mantle cell lymphoma
· Memory B cell - Burkitt’s cell leukaemia / Burkitt’s lymphoma
· Germinal centre B cell - Hodgkin’s Lymphoma
· IgM-secreting cell - Waldenstrom’s macroglobulinaemia
· Plasma cell - Multiple Myeloma
The same is not true for T-lymphocytes. There are essentially only two types of T-cell leukaemia; acute, representing malignancy of a thymocyte (pre-T cell) and chronic, which stems from adult T-cells. It is thought that the reason for this difference lies in the fact that in the various stages of T-cell development, cells apoptose in the absence of a signal in the thymus to positively select them. This short lifespan and pre-programmed death seems to be protective as the cells do not appear to have an opportunity to become malignant.
Lymphomas
Lymphomas are categorised into Hodgkin’s and non-Hodgkin’s on the basis of histological analysis. Non-Hodgkin’s lymphomas can be further categorised into T- or B- cell derived. Until relatively recently is was not known whether Hodgkin’s disease was of B- or T- origin. The cell central to Hodgkin’s disease is known as the Reed-Sternberg cell which is a very abnormal cell found on lymph node biopsy. It does not express either immunoglobulin or the T-cell receptor and so its origin was obscure. However DNA analysis of the RS cell demonstrated rearranged immunglobulin gene segments indicating a B-cell origin.